How Service Is Delivered To Long Term Care Facilities
Medicaid is the nation'southward major publicly-financed health insurance programme, covering the acute and long-term services and supports (LTSS) needs of millions of low-income Americans of all ages. With limited coverage under Medicare and few affordable options in the private insurance marketplace, Medicaid will continue to be the master payer for a range of institutional and community-based LTSS for people needing assistance with daily self-care tasks. Advances in assistive and medical engineering science that allow people with disabilities to exist more independent and to live longer, together with the crumbling of the babe boomers, will likely result in increased demand for LTSS over the coming decades. To reduce unmet need and curb public health care spending growth, state and federal policymakers will be challenged to find more efficient means to provide high quality, person-centered LTSS across service settings. This primer describes LTSS delivery and financing in the U.S., highlighting covered services and supports, types of care providers and care settings, beneficiary subpopulations, costs and financing models, quality improvement efforts, and recent LTSS reform initiatives.
What Are Long-Term Services and Supports?
"Long-term services and supports" encompasses the broad range of paid and unpaid medical and personal care assistance that people may need – for several weeks, months, or years – when they experience difficulty completing self-care tasks every bit a consequence of aging, chronic illness, or disability.
Long-term services and supports provide assist with activities of daily living (such as eating, bathing, and dressing) and instrumental activities of daily living (such as preparing meals, managing medication, and housekeeping). Long-term services and supports include, only are not limited to, nursing facility care, adult daycare programs, home wellness aide services, personal care services, transportation, and supported employment as well as assistance provided by a family caregiver. Intendance planning and care coordination services help beneficiaries and families navigate the health arrangement and ensure that the proper providers and services are in place to meet beneficiaries' needs and preferences; these services can exist essential for LTSS beneficiaries who often have substantial astute intendance needs as well.
Where Are Long-Term Services and Supports Provided and Past Whom?
Long-term services and supports are delivered in institutional and dwelling and customs-based settings.
These include institutions (such as nursing facilities and intermediate care facilities for individuals with intellectual disabilities) and domicile and community-based settings (such equally group homes or apartments).1 Over the last twenty years, there has been a shift toward serving more people in dwelling and community-based settings rather than institutions due in large part to the growth in beneficiary preferences for dwelling house and community-based services (HCBS) and states' obligations under the Supreme Court's Olmstead decision which found that the unjustified institutionalization of persons with disabilities violates the Americans with Disabilities Human action.2
Long-term services and supports are provided past unpaid family caregivers and by paid providers.
In the U.S., the majority of LTSS is provided by unpaid caregivers – relatives and friends – in home and community-based settings, allowing many with LTSS needs to age in place. Co-ordinate to a 2012 nationally representative survey, the majority of family caregivers are women age l and over who care for a parent for at to the lowest degree one year while maintaining outside employment.three This unpaid intendance ranges from help with getting to doctor appointments or paying bills to more intensive care such as profitable with bathing or wound care. As a person'due south daily intendance needs become more all-encompassing, paid LTSS delivered by straight care workers – medical professionals (such equally physicians or nurses) or para-professionals (such equally nurse aides or personal attendants) – may be required in addition to or in identify of family unit caregiver services.
Who Needs Long-Term Services and Supports?
Millions of Americans – children, adults, and seniors – demand to access long-term services and supports as a consequence of disabling weather and chronic illnesses.
People needing LTSS include elderly and non-elderly people with intellectual and developmental disabilities, physical disabilities, behavioral health diagnoses (such as dementia), spinal cord or traumatic encephalon injuries, and/or disabling chronic weather condition. A beneficiary's age, gender, socioeconomic status, living arrangement, and access to information most care options, in improver to his or her health and disability condition, can influence the types and amounts of LTSS utilized and the elapsing of care.4 , v People with electric current or future LTSS needs access information about available services and providers via information and referral networks (such as local Aging and Disability Resources Centers and Area Agencies on Aging) and outreach initiatives (such as peer-to-peer outreach in nursing home-to-community transition programs). The LTSS beneficiary population is growing more than racially and ethnically various, which has implications for ensuring cultural competency and language access in outreach, cess, care planning, and service commitment policies and practices.
Demographic trends suggest considerable growth in the number of Americans who will need LTSS in the coming decades.
Life expectancy remains relatively loftier, baby boomers continue to age into older adulthood, and advances in assistive and medical technology allow more people with chronic illnesses and disabling conditions to live longer and independently in the community. The number of elderly Americans is expected to more than than double in the next twoscore years (Figure 1). According to 2012 estimates, among people age 65 and over, an estimated 70 pct volition use LTSS, and people historic period 85 and over – the fastest growing segment of the U.S. population – are four times more than likely to need LTSS compared to people age 65 to 84.six , 7 Approximately seven in ten people historic period 90 and to a higher place have a disability, and among people between the ages of 40 and l, virtually one in ten, on average, volition have a disability that may require LTSS.8
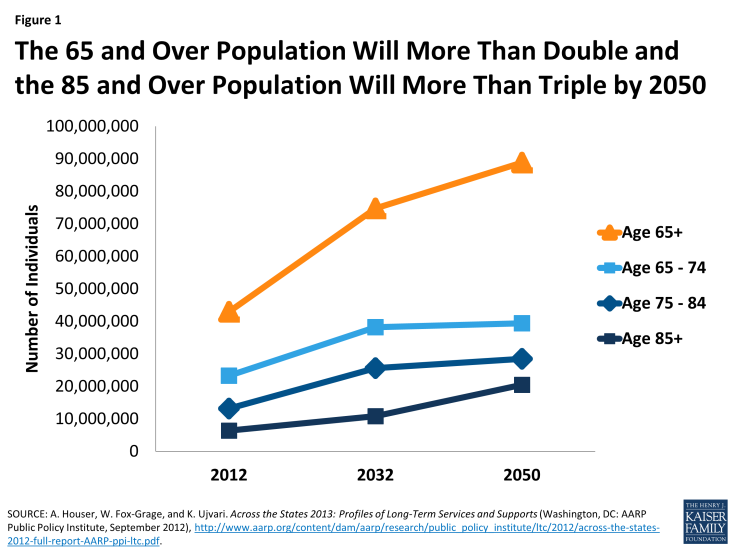
Figure one: The 65 and Over Population Volition More Double and the 85 and Over Population Will More than Than Triple by 2050
How Much Do Long-Term Services and Supports Cost and Who Pays For Them?
Long-term services and supports are expensive, with institutional care costs exceeding costs for home and customs-based services and supports.
Beyond unpaid care provided by relatives, LTSS costs often exceed what individuals and families can afford given other personal and household expenses. Institutional settings such as nursing facilities and residential care facilities are the about plush. In 2015, the median annual price for nursing facility care was $91,250.9 By and large, HCBS are less expensive than institution-based LTSS, but may still represent a major financial burden for individuals and their families. In 2015, the median cost for ane year of home health aide services (at $20/hour, 44 hours/week) was almost $45,800 and adult day care (at $69/24-hour interval, five days/calendar week) totaled almost $18,000 (Figure ii).ten
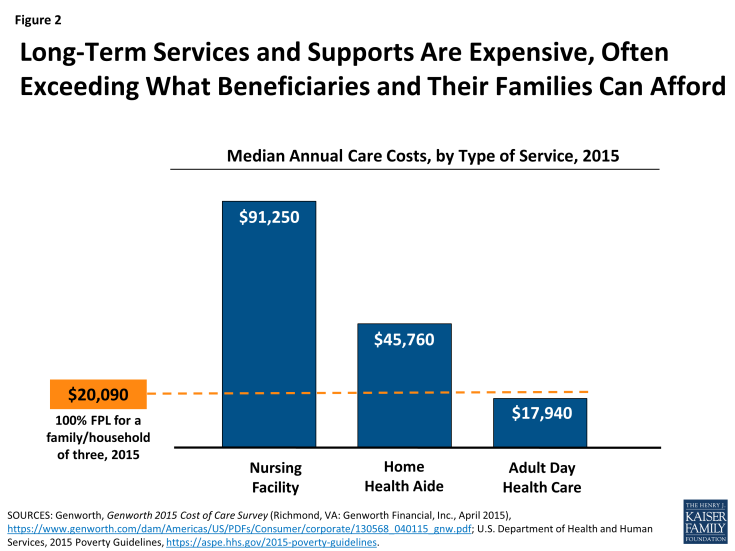
Figure two: Long-Term Services and Supports Are Expensive, Often Exceeding What Beneficiaries and Their Families Can Afford
Long-term services and supports are financed with individual and public dollars, with the bulk covered by publicly financed health insurance programs.
With few affordable options in the individual insurance market and limited coverage under Medicare, those with insufficient resources rely on Medicaid. According to the Centers for Medicare and Medicaid Services (CMS) National Health Expenditure Accounts data, total national spending on LTSS was $310 billion in 2013, with Medicaid covering 51 percent of total expenditures followed by other public,11 out-of-pocket spending, and private insurance (Effigy iii).
Medicaid is the primary payer for institutional and customs-based long-term services and supports. Medicaid, the nation's main public health insurance plan for people with low income, is administered past states within broad federal rules and financed jointly by states and the federal government. In 2013, Medicaid outlays for institutional and customs-based LTSS totaled just over $123 billion, accounting for nearly 28 percent of total Medicaid service expenditures that year.12 Medicaid eligibility, service commitment, financing, and the new and expanded HCBS options under the Affordable Care Human activity (ACA) are discussed below.
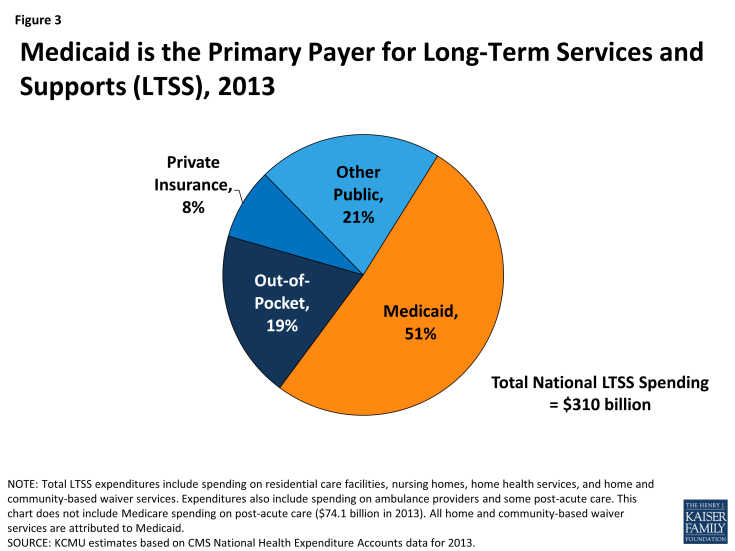
Figure 3: Medicaid is the Principal Payer for Long-Term Services and Supports (LTSS), 2013
Medicare coverage of long-term services and supports for seniors, nonelderly people with disabilities, and people with sure chronic conditions is limited. Medicare covers both acute intendance (such as physician visits) and postal service-astute services (such equally skilled nursing facility care) for people who have a qualifying work history and (1) are age 65 or older; (2) are nether age 65 and take been receiving Social Security Inability Insurance for more than 24 months; or (three) have end-stage renal disease or Amyotrophic Lateral Sclerosis.thirteen Nether Medicare, LTSS coverage is limited. Habitation health services are only covered for beneficiaries who are homebound, and personal intendance services are non covered by Medicare. Post-astute nursing facility care is covered for upwards to 100 days post-obit a qualified infirmary stay.
As of 2011, almost ten 1000000 beneficiaries – known as "dual eligibles" – were enrolled in both Medicaid and Medicare, with Medicaid paying for the majority of their long-term services and supports costs.xiv The dual eligible beneficiary population comprises seniors and younger people with disabilities who are entitled to Medicare and are also eligible for some level of assistance from their state Medicaid program. Medicare acts as the primary payer for a range of services for dual eligibles; Medicaid provides cost-sharing assistance and may pay for services not covered or limited nether Medicare.15 , 16 In 2011, 62 percent of Medicaid expenditures (or $91.8 billion) for dual eligibles were for LTSS.17 Under new waiver dominance in the ACA, selected states are testing models to align Medicare and Medicaid financing, seeking to better integrate and coordinate primary, acute, behavioral health, and LTSS for this vulnerable beneficiary population.xviii , 19
Private long-term care insurance is typically inaccessible to all with electric current or future care needs often due to high premium prices. Although private long-term care (LTC) insurance, which began equally nursing facility insurance, has been available for about 30 years, the market for this insurance production is relatively small. In 2011, 7 to 9 million Americans had private LTC insurance coverage and the boilerplate annual premium for an individual policy totaled $2,283.20 Paying for private LTC insurance can exist burdensome for individuals and families with express incomes; this is specially true for seniors who face higher premium costs while living on a stock-still income. Furthermore, the benefits are fourth dimension-limited, so consumers must estimate the amount of time they will require LTSS in the future, which may be difficult to do. Government back up for the buy of individual LTC insurance exists in the form of tax incentives and public-private partnerships between states and private insurance companies that let people with LTSS needs to access Medicaid services, subject to sure eligibility requirements, after purchasing and exhausting benefits under a state-qualified, private LTC insurance policy.21
Few individuals can afford to pay out-of-pocket for needed long-term services and supports, especially those living on stock-still incomes with limited personal savings and assets. In 2013, out-of-pocket spending accounted for 19 percentage of total national LTSS expenditures.22 A person'south ability to pay for electric current LTSS needs and/or save for futurity potential LTSS needs depends on many factors, including, just not limited to, wellness status, employment status and history, household income, debt and asset levels, and the availability of natural supports (such equally a family caregiver); unable to pay, individuals may delay or forego needed formal LTSS. Most seniors have limited resources, with seniors of color facing disproportionately college economical and health insecurity in retirement.23 In 2013, half of all Medicare beneficiaries, including seniors and younger adults with disabilities, had incomes below $23,500.24
What is Medicaid'southward Role in Long-Term Services and Supports Financing?
Medicaid Eligibility
People with long-term services and supports needs may authorize for Medicaid based solely on their low incomes or they may qualify at slightly higher incomes if they also meet disability-related functional criteria. Eligibility criteria vary by state, subject to certain federal minimum requirements. In improver, at land option, people whose income or assets exceed the threshold may later on qualify for Medicaid coverage by depleting financial resources, literally "spending down," to run across the financial eligibility criteria. People seeking Medicaid coverage for nursing facility intendance must contribute to the cost of care from their monthly income and are subject to an asset transfer review; the transfer of certain assets (such equally greenbacks gifts) inside the v-year "look dorsum" flow may outcome in a punishment and a period of ineligibility.25 To address the gaps in individual LTSS coverage and back up people with disabling conditions who desire to secure employment and live in the customs, many states opt to let workers with disabilities to have college incomes and "buy in" to Medicaid coverage by paying a monthly premium.26
Medicaid Long-Term Services and Supports
Within the Medicaid program, at that place has been a historical structural bias toward institutional intendance. States are required to cover nursing facility benefits, while coverage of most HCBS is optional.27 Equally a result, Medicaid HCBS spending patterns vary amid states, with states spending between 21 pct and 78 percent of their total Medicaid LTSS dollars on HCBS in 2013 (Figure 4).28 In add-on, the use of Medicaid HCBS versus institutional services varies beyond beneficiary subpopulations; in 2011, 80 percentage of nonelderly beneficiaries with disabilities used HCBS compared to 50 per centum of elderly beneficiaries (Figure 5).29
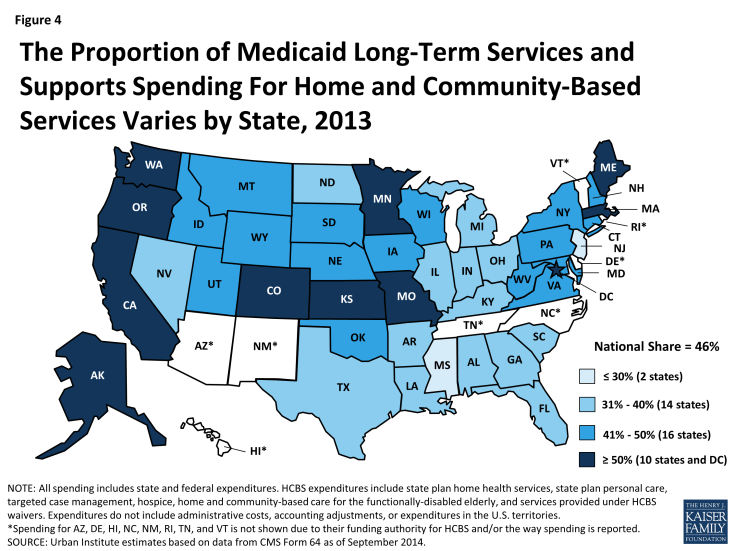
Figure four: The Proportion of Medicaid Long-Term Services and Supports Spending For Home and Community-Based Services Varies by Country, 2013
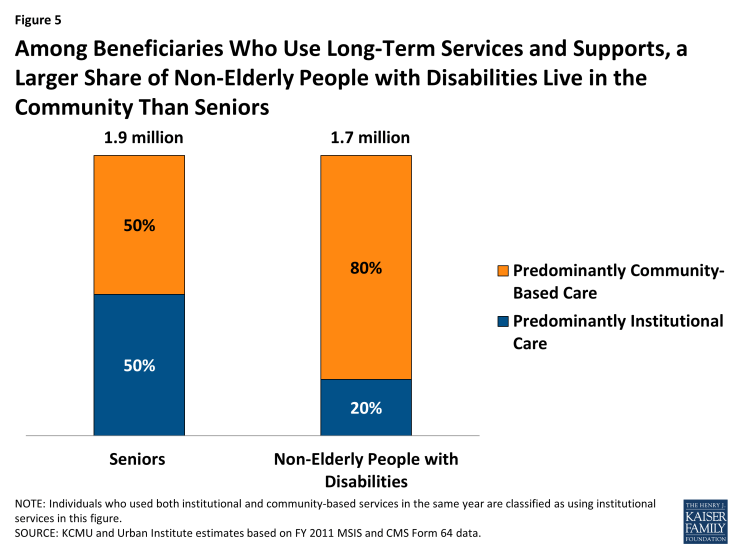
Figure 5: Among Beneficiaries Who Use Long-Term Services and Supports, a Larger Share of Non-Elderly People with Disabilities Live in the Community Than Seniors
There has been considerable progress in increasing the amount of Medicaid long-term services and supports dollars spent on community-based services and supports over the final 2 decades. In 2013, spending on HCBS accounted for 46 percent (or $56.6 billion) of full Medicaid LTSS spending, upwardly from 32 percentage (or $29.8 billion) in 2002.30 Three benefits account for the majority of Medicaid HCBS spending: (1) home health services, a mandatory land programme service; (2) personal intendance services, an optional state plan service; and (3) Section 1915(c) HCBS waivers, which allow states to waive certain federal requirements and provide HCBS to people who otherwise would have to access LTSS in an institutional setting. Just over 3.two million beneficiaries received home wellness, personal intendance, or home and community-based waiver services in 2011, with expenditures totaling $55.iv billion or only almost $17,200 per beneficiary.31 In addition, states can employ Section 1115 demonstration waivers to deliver HCBS, including through managed LTSS delivery systems (discussed below).32 The Medicaid program too provides authority for beneficiaries to self-direct their HCBS by decision-making the selection, training, and dismissal of providers and/or the allocation of their service budget.33
States have numerous options for funding Medicaid home and community-based services, including new and expanded options nether the Affordable Care Act.34 , 35 State implementation of the new and expanded HCBS options nether the ACA (i.e., Coin Follows the Person Sit-in, the Balancing Incentive Programme, the Department 1915(i) HCBS state plan option, and the Department 1915(k) Community First Choice state plan pick), some of which provide enhanced federal funding, was relatively slow through 2012. This was due, in part, to competing administrative and fiscal priorities inside state Medicaid programs.36 At that place is at present more widespread implementation of the options amid states, with numerous states pursuing multiple options either separately or in combination (Figure 6).
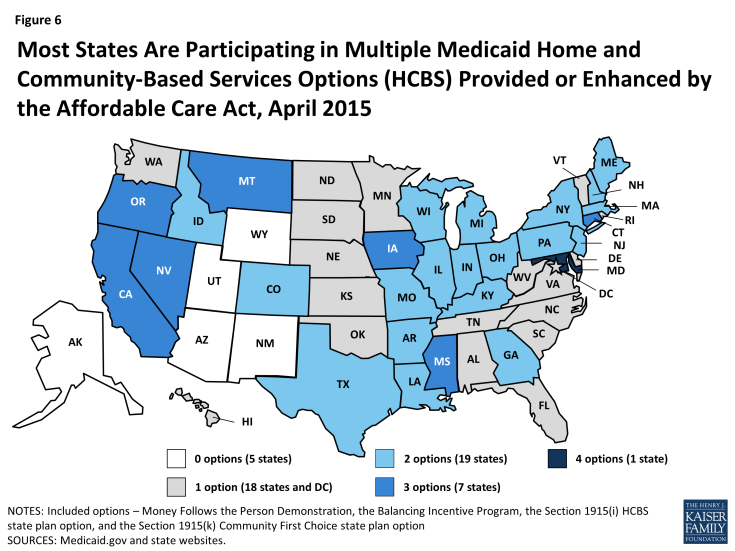
Figure vi: Almost States Are Participating in Multiple Medicaid Habitation and Customs-Based Services Options (HCBS) Provided or Enhanced by the Affordable Intendance Deed, April 2015
Section 1915(c) waivers accounted for the largest share of Medicaid home and community-based services enrollment and the majority of Medicaid dwelling house and community-based services spending in 2011. Expenditures for approximately 1.45 meg beneficiaries totaled $38.9 billion across 291 individual Section 1915(c) waiver programs. Non all who are eligible have admission to HCBS waiver services equally states may implement restrictive fiscal and functional eligibility standards, enrollment caps, service unit of measurement limits, or waiting lists in an effort to comprise costs. In 2013, there were over 536,000 individuals in 39 states on a Department 1915(c) waiver waiting list.37
Medicaid Commitment System Reforms
In that location has been increasing interest among states in transitioning from the traditional fee-for-service financial model to managed care to evangelize and coordinate services for Medicaid long-term services and supports beneficiaries. The number of states delivering and financing Medicaid LTSS via a risk-based capitated managed care model is expected to increase,38 and states as well are pursuing managed fee-for-service models, including primary care case direction. Managed care models, while relatively untested to date, offer potential opportunities for improving care coordination, and/or expanding admission to HCBS.39 Given the vulnerability of this casher population, it is important that managed LTSS systems are monitored to ensure access to the necessary services and supports on which beneficiaries rely to live independently in the community.
How is the Quality of Long-Term Services and Supports Evaluated?
Care standards and operation measures are important to inform country and national efforts to improve the quality of long-term services and supports delivered across care settings and service delivery models.
Ensuring timely access to high quality care for people with LTSS needs is a priority for beneficiaries and their families, service providers, and state and federal policymakers alike. However, quality measures for LTSS are not as well adult every bit those for intendance provided in clinical settings. In addition, LTSS operation measures tin can vary past state, prompting efforts to develop a core set of LTSS-specific quality measures to evaluate structural elements (such as provider staffing capacity), service delivery processes (such as timeliness of assessment), or care and performance outcomes (such as an improved ability to consummate a self-intendance task).40 , 41 Ongoing efforts to streamline assessment processes, improve reporting feedback mechanisms, and examine the effectiveness of LTSS-specific quality standards will exist vital to improving service commitment as the LTSS beneficiary population grows and becomes more diverse.
Quality in Institutional settings
Nursing homes certified to participate in the Medicare and Medicaid programs are regulated and must adhere to national and statewide quality balls and reporting standards, which were expanded by the Affordable Care Act. The ACA, which incorporates the Nursing Home Transparency and Comeback Act, the Elderberry Justice Human activity, and the Patient Safety and Abuse Prevention Human activity, is the outset comprehensive institutional care quality legislation since the 1987 Nursing Home Reform Act. The ACA requires CMS and nursing homes to implement provisions aimed at improving transparency and accountability, enforcement, and resident corruption prevention. For case, CMS must institute a national directly care worker payroll information collection and reporting organisation and add boosted facility-level staffing and complaint data to the Nursing Home Compare website,42 and nursing homes must disclose their ownership, management, and financing structures, implement compliance and ethics programs, meet CMS's quality assurance and improvement standards, and written report suspected crimes committed confronting residents to law enforcement regime. States and CMS continue to make progress in implementing the federal requirements as the provisions are expected to have a substantial impact on nursing home accountability for care quality.43
Quality in Abode and Community-Based Settings
As states keep to increase spending on home and community-based services equally an alternative to institutional intendance, work continues on developing specific quality measures to evaluate and improve dwelling house and community-based long-term services and supports. Improving and aligning quality standards across all Medicaid HCBS programs remains a priority for CMS, states, and stakeholders through initiatives such as measurement testing projects and educational activity and grooming opportunities for states and providers.44 With respect to Section 1915(c) waivers, the largest Medicaid HCBS program, CMS modified the quality assurance reporting system in 2014, with the goal of improving oversight of beneficiary outcomes and realigning land reporting requirements. Examples of ongoing efforts to identify or develop and evaluate HCBS quality measures include the Measure Applications Partnership/National Quality Forum,45 the Agency for Healthcare Research and Quality Medicaid Dwelling house and Customs-Based Services Measure out Scan,46 and the Long-Term Care Quality Alliance Quality Measurement Workgroup.47
Managed Long-Term Services and Supports and Quality
Given the growing interest amongst states in covering new populations and long-term services and supports benefits through risk-based, capitated managed care arrangements, monitoring beneficiaries' access to intendance and outcomes in these systems will remain important. In 2013, CMS issued guidance to states outlining best practices for designing and implementing managed LTSS programs with respect to quality measurement and other primal program elements. States implementing managed LTSS programs are expected to include a comprehensive quality strategy for assessing and improving care and quality of life for LTSS beneficiaries that aligns with existing Medicaid quality initiatives and systems.48
What Recent Efforts to Reform National Long-term Services and Supports Financing Accept Been Initiated?
Established past the Affordable Care Human action but later repealed earlier implementation, the Community Living Assist Services and Supports (CLASS) plan was designed to provide working adults the opportunity to first the costs of future long-term services and supports needs. 49 CLASS was intended to be a national, voluntary insurance program for purchasing LTSS coverage, financed by individual premium contributions, but concerns most solvency and adequacy of the cash benefit led to the plan's repeal by the American Taxpayer Relief Deed of 2013.50
Nether the aforementioned law that abolished the Community Living Assistance Services and Supports program, Congress established the time-express, federal, bipartisan Committee on Long-Term Care. The Committee's September 2013 Final Written report, outlines several service delivery, workforce, and financing policy recommendations, eastward.g., establishing integrated care teams, using technology-enhanced information sharing across intendance settings and among providers, training family caregivers, finding a sustainable residuum of public and private financing for LTSS.51 (Annotation: Five members of Commission later on issued an independent minority report which outlined alternative recommendations for LTSS reform.52) While the Commission recommended that time to come work be carried out through a national advisory commission,53 no such committee has been convened to date, although numerous public and individual stakeholders remain interested in advancing the national LTSS agenda.54 , 55
Looking Ahead
Reforming the nation's long-term services and supports system is likely to remain a topic of discussion in the coming decades every bit policymakers and other stakeholders consider options for coming together the growing demand for community-based options and addressing the lack of long-term services and supports coverage options outside of Medicaid. Given the significant public investment in the commitment and financing of LTSS, policymakers and other stakeholders have a vested interest in exploring LTSS reform options. In the absence of other feasible public or individual options to finance current and future LTSS needs for people of all ages, Medicaid will go along to be the major financing and delivery system for institutional and community-based LTSS for millions of Americans. Looking ahead, addressing community-based provider and housing shortages and streamlining admission to community-based care that supports functional independence and enhances quality of life will remain fundamental objectives of states' rebalancing efforts as the need for Medicaid HCBS continues to grow. Policymakers and other stakeholders too may focus on the condition of Medicaid initiatives to rebalance LTSS in favor of HCBS, with the expiration of Balancing Incentive Program funds in 2015, and Money Follows the Person funds in 2016. As the full general LTSS beneficiary population increases and becomes more various, country and federal governments and private stakeholders will be challenged to discover innovative ways to coordinate, deliver, and finance high quality, person-centered LTSS in the most appropriate care setting that promotes health and well-being, respects casher preferences and rights, and maximizes efficiency to manage cost growth.
How Service Is Delivered To Long Term Care Facilities,
Source: https://www.kff.org/medicaid/report/medicaid-and-long-term-services-and-supports-a-primer/
Posted by: andinoalearand.blogspot.com


0 Response to "How Service Is Delivered To Long Term Care Facilities"
Post a Comment